来源:发布时间:2021-04-11编辑:校对:审核:点击: 次


目前,没有大数据的医学研究证明天气变化和关节疼痛具有统计学相关性。
2017年,BMJ杂志(IF:30.223)发表了一篇文章,美国一个医学团队分析了4年之间近155.3万名年龄大于 65 岁有关节痛或背痛患者(包括类风湿关节炎、骨关节炎、脊椎病、椎间盘疾病和其他非创伤性关节疾病患者)的门诊记录,比较了患者在雨天和非雨天之间关节或腰痛的就诊比例。
结论认为,关节痛/背痛与下雨天可能并不存在因果关系,尤其是人们最常担心的类风湿关节炎的疼痛与下雨天未发现相关性。
但是,作者也提出了假设:人类的大脑擅长发现所谓的“规律”,可能患者下雨天和晴天关节疼痛的频率相同,但是下雨天前后刚好痛了,并且下雨天的就诊经历更困难,容易给人留下印象,人们可能就会一直记在脑海中。


有一个体征叫做“凉髌征”,膝关节附近脂肪少、保温性能较差,膝关节温度较低,再加上阴雨天气,气温和气压都会出现明显变化,可能病变关节的关节周血管收缩,软组织紧张僵硬,关节内炎性介质和关节积液不能很好地被吸收排出,从而导致关节的僵硬、不适、疼痛感。这可能是阴雨天气关节疼痛、关节不适的原因。
临床观察显示,天气变化时膝盖疼的主诉似乎更多出现在骨关节炎、类风湿关节炎的患者口中。


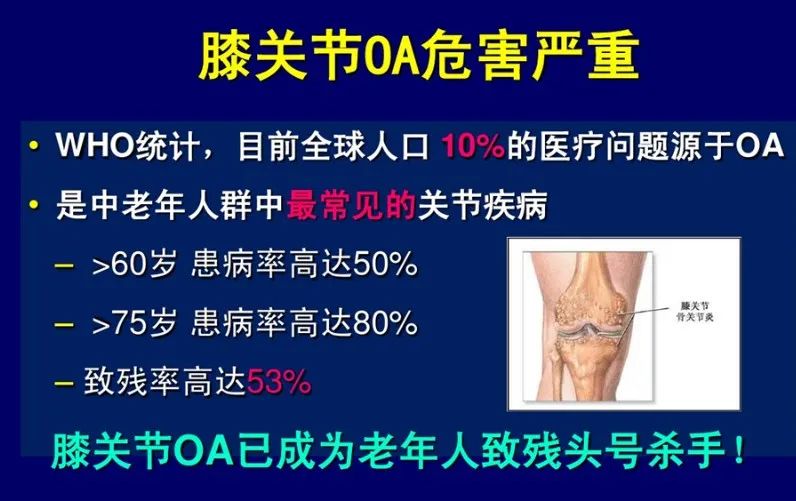
骨关节炎(OA)是中老年最常见的慢性关节疾病之一,女性发病率高于男性,呈现明显地区差异,农村地区膝关节症状性骨关节炎患病率高于城市地区,也常见于重体力劳动者、运动员、肥胖人群。
骨关节炎是由多种因素引起关节软骨纤维化、皲裂、溃疡、脱失、骨赘形成的以关节疼痛为主要症状的退行性疾病。累及部位包括膝、髋、踝、脊柱(颈椎、腰椎)等承重关节和远指间关节。以关节疼痛、关节弹响为主要临床表现,同时可伴有晨起时关节及其周围僵硬感(简称晨僵)(多小于1小时)、关节肿大、骨擦音以及关节活动受限,晚期可出现关节畸形等。
骨关节炎主要采取生活方式改变、锻炼康复及控制体重等治疗,同时给予非甾体类消炎止痛、硫酸氨基葡萄糖、双醋瑞因等药物治疗,对于晚期骨关节炎、关节畸形患者,可根据个体需求采取关节置换术治疗。

类风湿关节炎(RA)好发于青中年女性,女性发病率高于男性,发病可能跟感染、遗传、内分泌因素相关。
类风湿关节炎是以侵袭性、对称性多关节炎为主要临床表现的慢性、全身性自身免疫性疾病。基本病理改变为关节滑膜的慢性炎症、血管翳形成,并逐渐出现关节软骨和骨破坏,最终导致关节畸形和功能丧失。
类风湿关节炎临床症状包括晨僵(多大于1小时)、关节红肿热痛、关节畸形,关节外受累者可能出现类风湿结节(多位于关节隆突部及受压部位的皮下)、血管炎(通常见于长病程、血清类风湿因子阳性且病情活动的病人,可表现为瘀点、紫癜、指/趾坏疽、梗死等),还可能出现神经、心脏、非受累相关的症状。实验室检查可能出现类风湿因子、抗环瓜氨酸肽抗体、抗角蛋白抗体的阳性,C反应蛋白、血沉升高。
类风湿关节炎主要使用抗风湿药、糖皮质激素、生物制剂控制疾病,目前尚无根治疗法。


关节痛可能由多种原因导致,没有经过系统的学习和长期的临床实践,非医疗人士难以通过简单的症状诊断。而关节痛、风湿病是虚假医疗小广告的重灾区,不少患者听信传言、广告,胡乱用药。
建议出现关节晨僵、红肿热痛的患者,至风湿免疫科门诊就诊,专科医生通过详细询问病史、查体和辅助检查,明确诊断,方能对症下药,切不可道听途说、自行用药、拖延诊治。


Jena AB, Olenski AR, Molitor D, et al. Associationbetween rainfall and diagnoses of joint or back pain: retrospective claimsanalysis. BMJ. 2017。
Objective: To study the relation between rainfall and outpatient visits for joint or back pain in a large patient population.
Design: Observational study.
Setting: US Medicare insurance claims data linked to rainfall data from US weather stations.
Participants: 1 552 842 adults aged ≥65 years attending a total of 11 673 392 outpatient visits with a general internist during 2008-12.
Main outcome measures: The proportion of outpatient visits for joint or back pain related conditions (rheumatoid arthritis, osteoarthritis, spondylosis, intervertebral disc disorders, and other non-traumatic joint disorders) was compared between rainy days and non-rainy days, adjusting for patient characteristics, chronic conditions, and geographic fixed effects (thereby comparing rates of joint or back pain related outpatient visits on rainy days versus non-rainy days within the same area).
Results: Of the 11 673 392 outpatient visits by Medicare beneficiaries, 2 095 761 (18.0%) occurred on rainy days. In unadjusted and adjusted analyses, the difference in the proportion of patients with joint or back pain between rainy days and non-rainy days was significant (unadjusted, 6.23% v 6.42% of visits, P<0.001; adjusted, 6.35% v 6.39%, P=0.05), but the difference was in the opposite anticipated direction and was so small that it is unlikely to be clinically meaningful. No statistically significant relation was found between the proportion of claims for joint or back pain and the number of rainy days in the week of the outpatient visit. No relation was found among a subgroup of patients with rheumatoid arthritis.
Conclusion: In a large analysis of older Americans insured by Medicare, no relation was found between rainfall and outpatient visits for joint or back pain. A relation may still exist, and therefore larger, more detailed data on disease severity and pain would be useful to support the validity of this commonly held belief.
内容来源:风湿免疫科
 返回顶部
返回顶部